Postpartum Haemorrhage
- Home
- Postpartum Haemorrhage
Postpartum haemorrhage (PPH) is excessive bleeding after childbirth, one of the leading causes of maternal morbidity and mortality worldwide. PPH is defined as blood loss exceeding 500 milliliters following vaginal delivery or 1,000 milliliters after a cesarean section. Although some bleeding is normal, PPH requires immediate medical intervention to prevent shock and life-threatening complications. Early recognition and treatment are crucial for the health and safety of the mother.
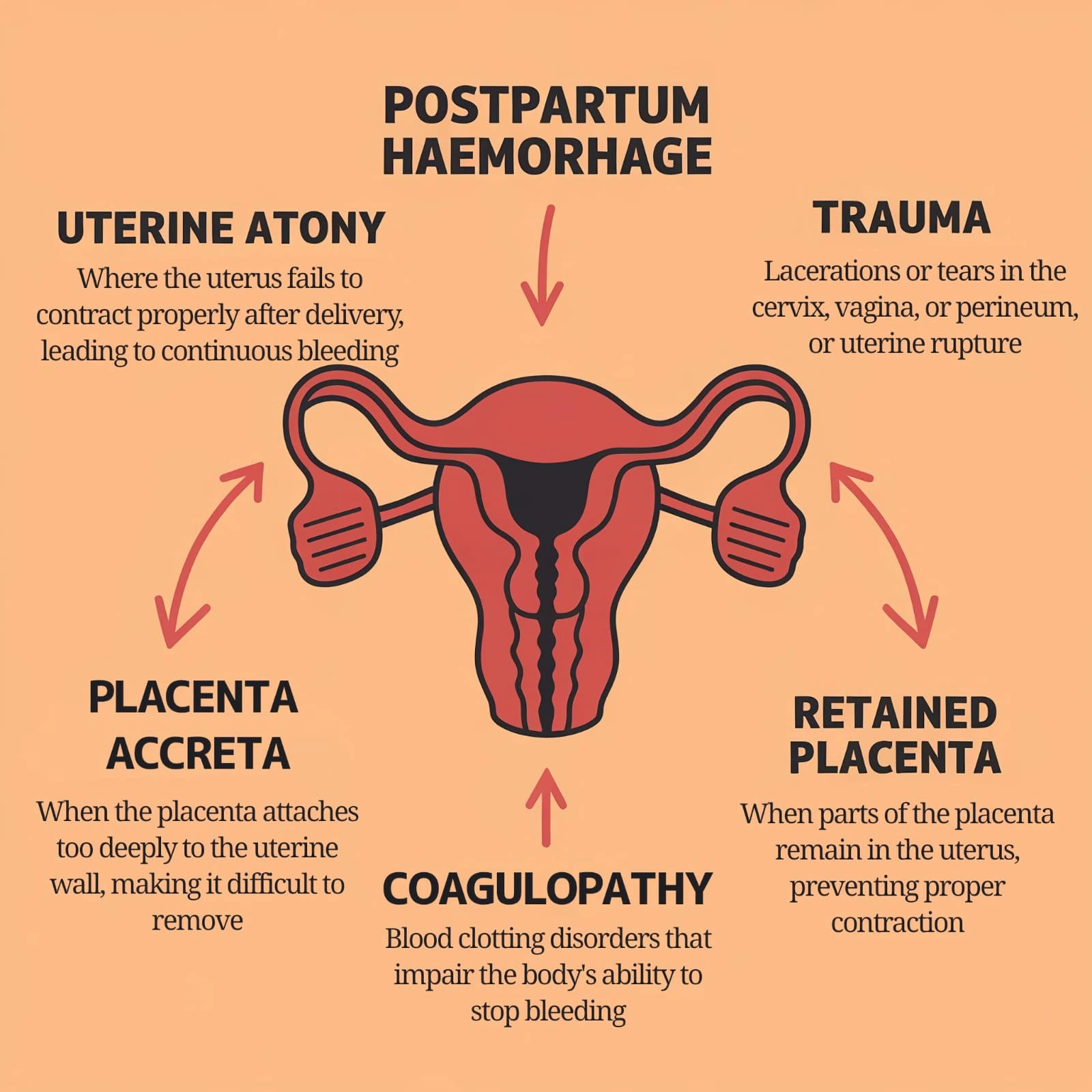
Causes of Postpartum Haemorrhage
PPH can be classified into primary (within the first 24 hours) and secondary (after 24 hours, within six weeks postpartum). The common causes include:
- Uterine Atony: The most common cause, where the uterus fails to contract properly after delivery, leading to continuous bleeding.
- Trauma: Lacerations or tears in the cervix, vagina, or perineum, or uterine rupture.
- Retained Placenta: When parts of the placenta remain in the uterus, preventing proper contraction.
- Placenta Accreta: When the placenta attaches too deeply to the uterine wall, making it difficult to remove.
- Coagulopathy: Blood clotting disorders that impair the body’s ability to stop bleeding.

Symptoms of Postpartum Haemorrhage
The symptoms of PPH include:
- Heavy Bleeding: Vaginal blood loss that exceeds normal post-delivery amounts.
- Tachycardia: Rapid heart rate due to blood loss.
- Hypotension: Low blood pressure, often leading to shock.
- Pale or Cool Skin: Indicating poor circulation due to blood loss.
- Weakness and Dizziness: Resulting from blood volume loss.
- Restlessness: Anxiety and agitation due to reduced oxygen supply to the body
Primary PPH occurs within 24 hours, while secondary PPH is noticed later, particularly if the placenta has not been fully expelled.
Benefits of Early Treatment
Timely identification and treatment of PPH are crucial to preventing severe complications, including:
- Faster Stabilization: Quick management reduces the risk of shock and further blood loss.
- Preservation of Fertility: Proper treatment can avoid hysterectomy, preserving the ability to have future pregnancies.
- Prevention of Further Complications: Early intervention prevents complications like infection or coagulopathy (DIC).
Latest Treatment Techniques for Postpartum Haemorrhage
The treatment for PPH depends on its cause and severity. Key treatment options include:
1. Uterine Massage and Uterotonic Medications
Uterine massage is the first-line treatment for uterine atony, which helps stimulate contractions. Medications like oxytocin, misoprostol, and ergometrine are administered intravenously or intramuscularly to promote uterine contractions and stop bleeding.
Example: After a vaginal delivery, Maria experienced heavy bleeding. Her doctor administered oxytocin and performed uterine massage, helping to stop the bleeding.

2. Surgical Interventions
If uterine massage and medications fail, surgical procedures may be required:
- B-Lynch Suture: A compression suture technique used to control bleeding by compressing the uterus.
- Hysterectomy: In severe cases where other treatments fail, removing the uterus may be necessary to save the mother’s life.
Example: Jane developed severe bleeding after a cesarean section. Despite using uterotonic medications, the bleeding persisted. A B-Lynch suture was successfully applied to stop the hemorrhage.
3. Balloon Tamponade
A balloon tamponade is inserted into the uterus and inflated to apply pressure to stop the bleeding. This temporary solution controls blood flow from the uterine arteries until further interventions can be done.
Example: Sarah’s PPH was caused by uterine atony. A balloon tamponade was inserted, stabilizing her condition until additional treatment could be performed.
4. Arterial Embolization
Arterial embolization involves blocking the arteries that supply blood to the uterus. This method is used when other treatments fail and can help prevent the need for a hysterectomy.
Example: Emily’s case of PPH required arterial embolization. Despite medical treatment, bleeding continued, and embolization effectively stopped the bleeding, avoiding further complications.
Conclusion
Postpartum hemorrhage is a critical condition that requires prompt treatment to avoid severe complications and ensure the mother’s safety. The latest techniques, including uterine massage, uterotonic medications, balloon tamponade, and arterial embolization, offer effective solutions for managing PPH. Early detection and intervention are vital for improving outcomes and preserving maternal health.
If you experience heavy bleeding or other symptoms of PPH after childbirth, seek immediate medical attention to ensure proper care and treatment.
Frequently Asked Questions (FAQs)
PPH can be caused by uterine atony, trauma, retained placenta, placenta accreta, and coagulopathy.
Treatments include uterotonic medications, uterine massage, balloon tamponade, arterial embolization, or surgery (such as B-Lynch sutures or hysterectomy).
Yes, if untreated, PPH can lead to shock, organ failure, or death. Early treatment is crucial for preventing complications.
Symptoms include excessive bleeding, low blood pressure, rapid heart rate, dizziness, and cool or pale skin.
Would you like to request an appointment?
You can call on +91-98200 86520 for Appointments or fill the form below
If you have recently given birth and are experiencing any signs of excessive bleeding, don’t wait. Contact us immediately to schedule a consultation and get the treatment you need to ensure your health and well-being.
