Pre-operative Embolization
- Home
- Pre-operative Embolization
Interventional oncology is a subspecialty field of Vascular interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments (e.g. biopsy needles, ablation electrodes, intravascular catheters) to allow targeted and precise treatment of solid tumours located in various organs of the human body.
While the surgical resection of tumours is generally accepted to offer the best long-term solution, it is often not possible due the size, number or location of the tumour. Vascular Interventional Radiology therapies may be applied to shrink the tumour, making a surgical or interventional treatment possible.

Patients can greatly benefit from Interventional Oncology treatments. The minimally invasive nature of the treatments means they cause less pain, fewer side effects and shorter recovery times. Many of these procedures can be performed on an outpatient basis, thereby reducing costs.
Pre-operative Embolization:
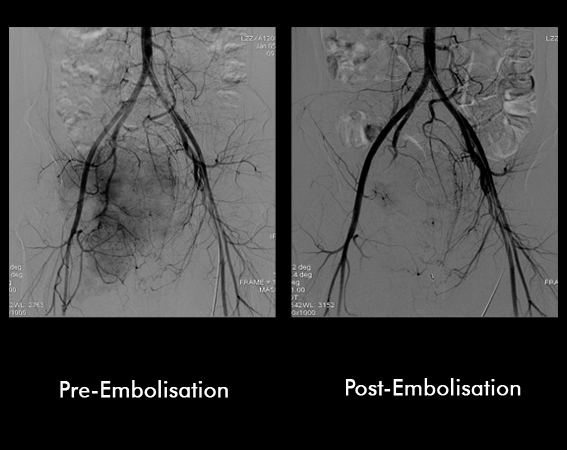
The surgical removal of a tumour can often be made easier if the blood supply to the mass is decreased prior to surgery. Planned blockage of the blood vessels (embolization) decreases the amount of bleeding encountered by the surgeon, which in turn decreases the need for blood transfusions and typically decreases the duration of the operation.
An embolization is a procedure in which a catheter is placed into an artery (usually in the leg, like for an angiogram of the heart) and carefully navigated into the blood vessels supplying the tumour under X-ray guidance. An angiogram is obtained by injecting X-ray dye into the blood vessel to examine the blood supply of the tumour and verify that it is safe to eliminate that vessel. Material is then injected through the catheter to block the blood vessel. This procedure is typically performed within a few days of planned surgery for maximum benefit.
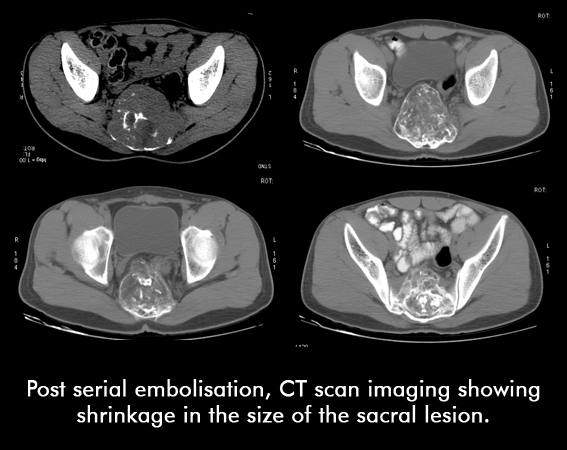
22 yr non married female presented with pain in the lower back radiating to both the hips. Patient was not able to walk. On CT scan, there was a large mass involving the sacrum, which was proven to be a Giant Cell Tumour on Biopsy. Patient underwent serial episodes of Embolisation.