Liver Cancer (TACE)
- Home
- Liver Cancer (TACE)
Interventional oncology is a subspecialty field of Vascular interventional radiology that deals with the diagnosis and treatment of cancer and cancer-related problems using targeted minimally invasive procedures performed under image guidance. Interventional oncology has developed to a separate pillar of modern oncology and it employs X-ray, ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) to help guide miniaturized instruments (e.g. biopsy needles, ablation electrodes, intravascular catheters) to allow targeted and precise treatment of solid tumours located in various organs of the human body.
While the surgical resection of tumours is generally accepted to offer the best long-term solution, it is often not possible due the size, number or location of the tumour. Vascular Interventional Radiology therapies may be applied to shrink the tumour, making a surgical or interventional treatment possible.

Patients can greatly benefit from Interventional Oncology treatments. The minimally invasive nature of the treatments means they cause less pain, fewer side effects and shorter recovery times. Many of these procedures can be performed on an outpatient basis, thereby reducing costs.
Trans-arterial Chemoembolization (TACE) and Radio-embolization:
Embolization is a procedure that injects substances to try to block or reduce the blood flow to cancer cells. Embolization is an option for some patients with tumours that cannot be removed by surgery. It can be used for tumours that are too large to be treated with ablation (usually larger than 5 cm across). In this procedure a catheter (a thin, flexible tube) is put into an artery through a small cut in the inner thigh and threaded up into the hepatic artery in the liver. A dye is usually injected into the bloodstream at this time to help the doctor monitor the path of the catheter via angiography, a special type of x-ray. Once the catheter is in place, small particles are injected into the artery to plug it up.
TACE is a combination therapy of Trans-arterial embolization and regional chemotherapy. Chemoembolization delivers a high dose of cancer-killing drug (chemotherapy) directly to the organ while depriving the tumour of its blood supply by blocking (embolizing) the arteries feeding the tumour. This combination of embolotherapy and regional chemotherapy has synergistic, anti-tumour effects. Another added benefit is that the use of combination therapy results in lower systemic drug levels and therefore less toxicity.
Embolization can also be combined with radiation therapy and this is known as trans-arterial radioembolization.
This is done by injecting small beads (called microspheres) that have a radioactive isotope (yttrium-90) stuck to them. Once infused, the beads lodge in the blood vessels near the tumour, where they give small amounts of radiation to the tumour site for several days. The radiation travels a very short distance, so its effects are limited mainly to the tumour.
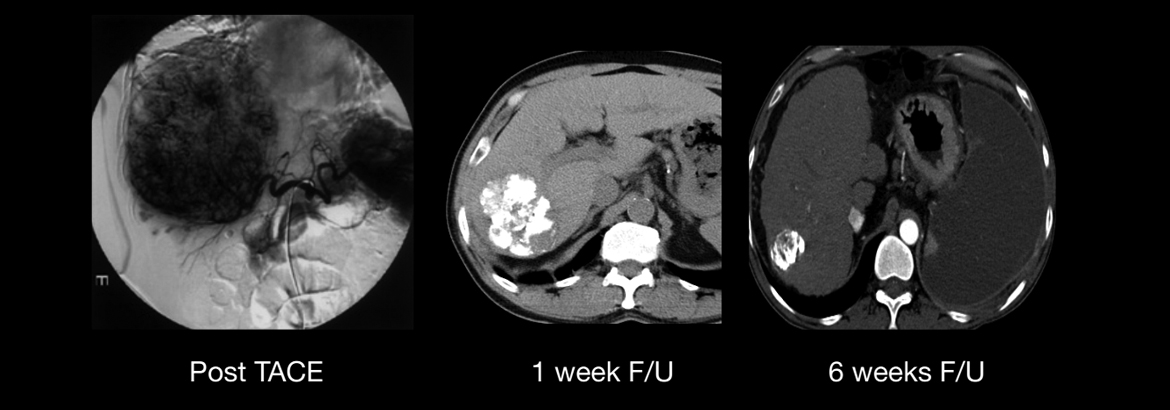
Case - 1 :
52yr old male patient, Known case of HBsAg positive induced multicentric bi-lobar Hepatocellular Carcinoma. Patient is inoperable and was suggested Palliative Chemotherapy.Multiple sessions of Transarterial Chemoembolisation (TACE) were done.