Gastrointestinal Bleeding
- Home
- Gastrointestinal Bleeding
Gastrointestinal bleeding (GI bleeding) is a serious medical condition that involves bleeding within the digestive tract. It can occur anywhere from the mouth to the rectum, ranging from mild to severe. Understanding the causes, symptoms, and treatment options is crucial for effective management. This guide explores the latest treatments and offers practical insights for individuals seeking help with gastrointestinal bleeding.
Causes of Gastrointestinal Bleeding
GI bleeding can stem from various causes, often linked to underlying medical conditions. Here are the most common causes:
- Peptic Ulcers: Sores that develop in the stomach lining or the upper part of the small intestine, often caused by H. pylori bacteria or long-term use of non-steroidal anti-inflammatory drugs (NSAIDs).
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux can lead to bleeding in the esophagus.
- Diverticular Disease: Small pouches that form in the colon and can become inflamed or bleed.
- Cancers: Malignant tumors in the stomach, colon, or rectum can cause bleeding.
- Hemorrhoids and Anal Fissures: These are common causes of rectal bleeding, usually not associated with more serious conditions.
- Varices: Swollen veins in the esophagus or stomach, often seen in people with liver disease, can rupture and lead to severe bleeding.

Symptoms of Gastrointestinal Bleeding
The symptoms of GI bleeding vary depending on the location and severity of the bleeding. Common signs include:
- Black, tarry stools (melena), which indicate bleeding from the upper digestive tract.
- Bright red blood in stool or vomit (hematochezia), suggesting bleeding from the lower digestive tract.
- Abdominal pain or cramps.
- Fatigue or weakness due to blood loss.
- Dizziness or fainting, often caused by significant blood loss.
Benefits of Early Treatment
Early diagnosis and intervention are crucial to prevent complications like severe blood loss or shock. Timely treatment can lead to:
- Faster Recovery: Early medical intervention ensures quicker stabilization and reduces the risk of long-term damage.
- Avoidance of Severe Complications: Addressing the source of the bleeding early can prevent life-threatening conditions such as anemia, shock, or organ failure.
- Better Outcomes: With modern medical techniques, outcomes for GI bleeding are much improved when treated promptly.
Latest Treatment Techniques for Aortic Aneurysm and Aortic Dissection
Advancements in medical technology have provided effective, minimally invasive treatments for gastrointestinal bleeding. Some of the most commonly used techniques include:
1. Endoscopic Treatment:
- Endoscopic Hemostasis: A procedure where an endoscope is used to locate the source of the bleeding, followed by cauterization, clipping, or injection of hemostatic agents to stop the bleeding.
- Endoscopic Variceal Ligation: This technique is used to treat varices in the esophagus and stomach by placing rubber bands around the swollen veins to stop the bleeding.
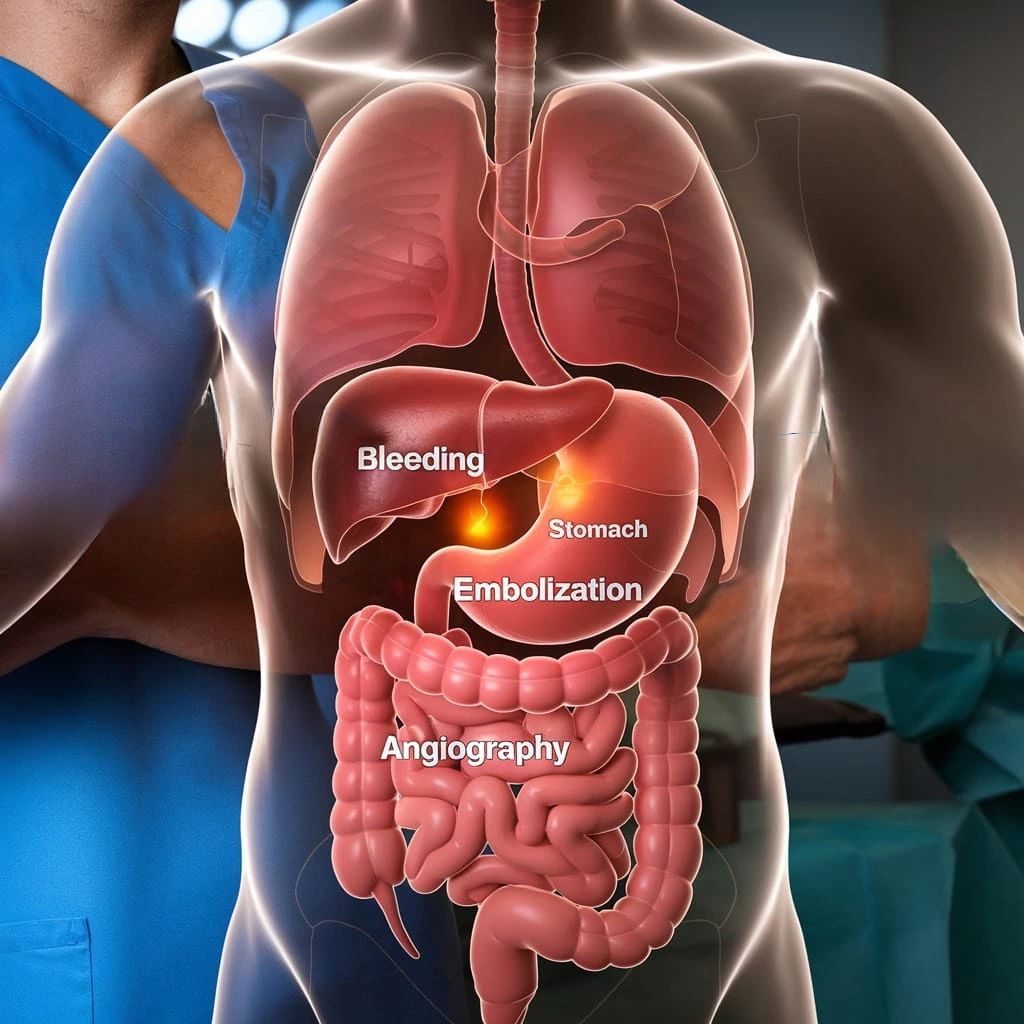
2. Angiography and Embolization:
In cases where endoscopy isn’t sufficient, angiography is used to identify bleeding vessels. These vessels are then embolized (blocked) using a variety of materials like coils or glue to control the bleeding.

3. Surgical Treatment:
Surgery is considered in severe cases or when other treatments fail. Procedures may involve removing a portion of the affected digestive organ or repairing damaged blood vessels.
4. Medications
- Proton Pump Inhibitors (PPIs): Used to reduce stomach acid, which helps heal ulcers and reduce bleeding.
- Somatostatin Analogs: Often used to manage variceal bleeding by reducing blood flow to the affected area.
Conclusion
Gastrointestinal bleeding is a serious condition, but with proper diagnosis and modern treatment options, it is highly manageable. Early intervention is key to preventing complications and improving patient outcomes. If you experience symptoms of GI bleeding, seeking medical advice promptly is crucial for effective treatment.
Frequently Asked Questions (FAQs)
Common causes include peptic ulcers, GERD, diverticular disease, and cancers. Hemorrhoids and anal fissures are also frequent causes of bleeding.
Diagnosis typically involves endoscopy, imaging tests like angiography, and blood tests to assess the extent of bleeding.
While it can be serious, especially if left untreated, most cases are manageable with early intervention and appropriate treatment.
While not all cases are preventable, lifestyle changes such as avoiding excessive use of alcohol, managing stress, and treating underlying conditions like GERD can help reduce the risk.
It’s important to seek medical attention immediately. Blood in stool can be a sign of gastrointestinal bleeding and requires prompt evaluation by a healthcare professional.
Would you like to request an appointment?
You can call on +91-98200 86520 for Appointments or fill the form below
If you’re experiencing symptoms of brain vascular issues, contact us today to schedule a consultation and explore your treatment options. Early diagnosis can prevent serious complications and improve your health outcomes.
